From Premiums to Utilization: Where to Find Cost-Saving Opportunities in Your Benefits Plan
- Published Date: August 22, 2025
Rising healthcare costs are no longer a surprise—they’re a constant. But knowing that spend is increasing isn’t the same as knowing why. For organizations providing insurance to employees, the key to unlocking real savings lies in visibility: not just into premiums, but into how benefits are actually used.
Total Rewards Analytics (TRA) helps benefits leaders move from surface-level insights to deep cost intelligence. By examining utilization trends, claim drivers, and plan design effectiveness, TRA reveals where costs are coming from—and where interventions can have the greatest impact.
The Real Cost Drivers Are Often Hidden
Many organizations track top-line expenses like premiums, but miss the cost implications of how care is accessed. For instance:
- Are high-cost claims driven by chronic conditions or avoidable ER visits?
- Is pharmacy spend rising due to specialty medications or generic underuse?
- Are certain demographics using fewer preventive services—leading to higher long-term costs?
Without a detailed breakdown of claims and utilization patterns, companies are left reacting to costs rather than managing them.
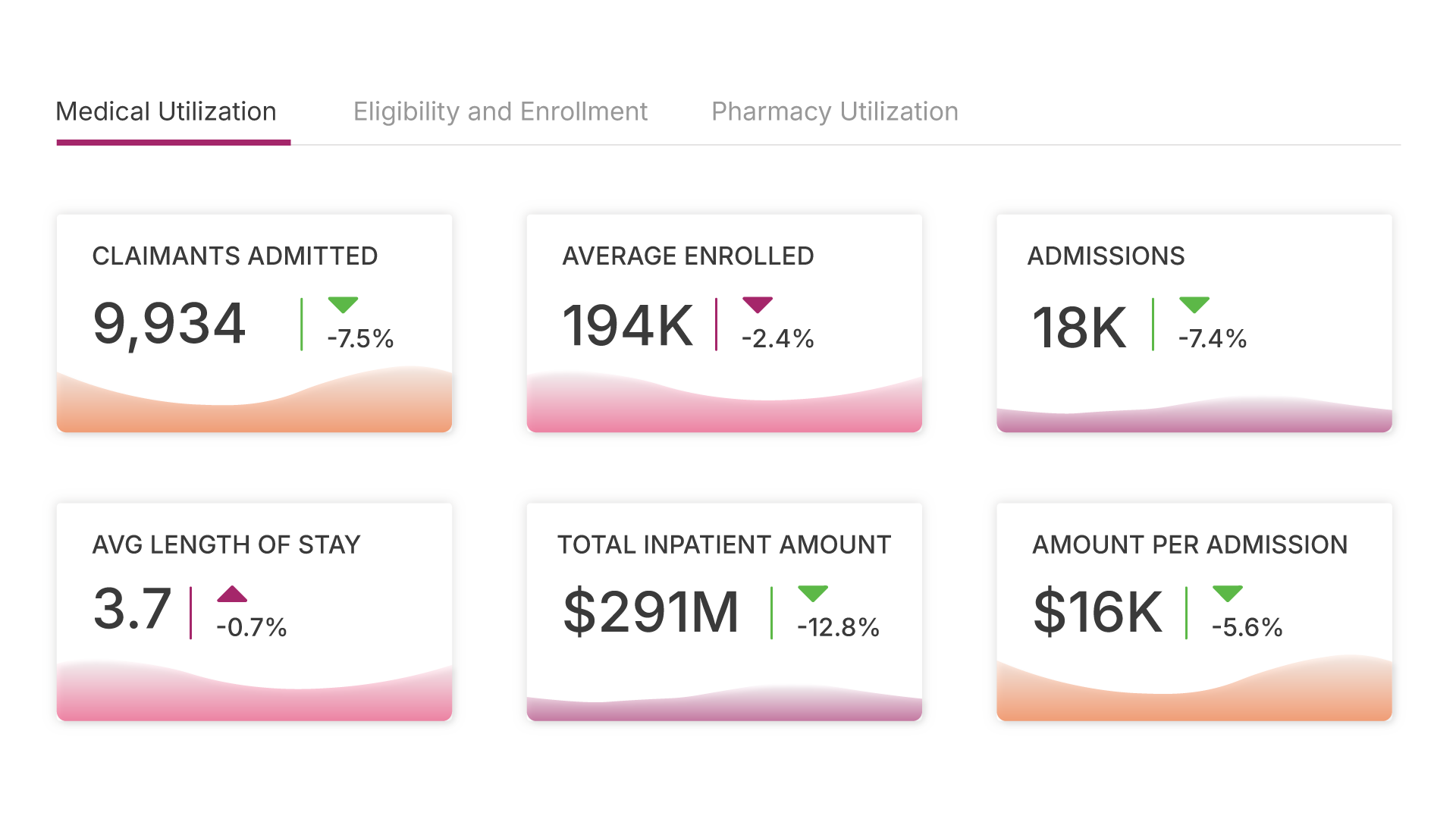
What TRA Makes Visible
A modern Total Rewards Analytics platform unifies claims data from multiple vendors and standardizes it for real-time, apples-to-apples analysis. This means benefits teams can:
- Track utilization by service type, demographic, or geography
- Drill into pharmacy claims to identify high-impact drug categories
- Benchmark costs against similar organizations or internal goals
- Pinpoint low engagement in preventive or wellness programs
The result: clearer insights, smarter interventions, and greater accountability across the benefits ecosystem.
Finding Opportunities to Save
When organizations can see clearly, they can act decisively. Some of the most common opportunities uncovered through TRA include:
- Plan redesigns that encourage preventive care or lower-cost providers
- Targeted communications to improve program engagement among underutilizing populations
- Chronic condition management programs tailored to specific claims trends
- Pharmacy benefit adjustments that control specialty spend without hurting outcomes
These aren’t theoretical improvements—they translate into real financial impact and improved employee wellbeing.
Explore how TRA surfaces cost-saving opportunities through utilization analytics.
Our TRA Suite surfaces critical trends—from rising healthcare costs to shifting utilization patterns—via pre-configured dashboards.
See how usage patterns reveal what’s driving your healthcare spend.
Strategic Cost Control, Not Just Cuts
Cost savings don’t have to come from reducing coverage. In fact, many of the most effective strategies involve smarter investments: in early detection, employee education, or plan configurations that meet employees where they are.
TRA empowers HR and finance teams to make those strategic decisions with confidence—because the data tells the full story.
Conclusion: Don’t Just Manage Costs—Understand Them
With the right analytics, companies can shift from reacting to rising healthcare costs to proactively managing them. Total Rewards Analytics helps connect the dots—from premiums to utilization—so organizations can find savings without sacrificing impact.
In a world where every healthcare dollar counts, insight isn’t a luxury. It’s a competitive advantage.
Explore the Latest
Insights, stories, and trends shaping the future of work and rewards.